Rising to new challenges – a blog by Sue Stockdale, Trainee Advanced Nurse Practitioner
I am a Trainee Advanced Nurse Practitioner at NIHR Manchester Clinical Research Facility (CRF). I am based at Wythenshawe Hospital, which is part of Manchester University NHS Foundation Trust (MFT).
Advanced Nurse Practitioners (ANPs) come from a range of professions including nursing, paramedics, physiotherapy, pharmacy and dieticians. They have a high level of autonomy in the assessment, diagnosis and treatment of patients, and this requires advanced clinical decision-making skills.
As a Research Nurse Manager at Manchester CRF, I wanted to further my career in a role where I could develop my clinical and research skills and retain patient contact – which drew me to the ANP role. Also, driving forward the service that we provide at the CRF excited me, as I could visualise how the addition of an ANP at our facility at Wythenshawe Hospital could help improve service delivery through increased capability and capacity, ultimately resulting in more patients accessing clinical trials.
I’m very keen to expand my knowledge by undertaking the necessary master’s degree training, and further consolidate this knowledge through practical clinical experience. Clinical practice makes up only 25 per cent of the four pillars that underpin the ANP role, with the remaining three being leadership & management, education, and research. With directed training and clinical support from the CRF, I feel that I can rise to the challenges of all four pillars, which will provide a framework around which my research ACP role can be developed.
Training to become an Advanced Nurse Practitioner in a global pandemic
The master’s programme for ‘Advanced Clinical Practice’ is delivered at universities throughout the country. My programme is carried out over two years, with two academic days per week and three days spent in clinical practice. The academic content itself is very intense, with 400 hours of study in the first semester alone. As a mature student, this has at times been a sobering thought. Qualified ANPs who have made it to the other side have reassured me that this is normal and despite the intensity, I do enjoy the academic step-up. As an avid runner, I use my running time as a way of relaxing and clearing my mind, ready for the next academic session. I’m continually reminding myself that my ANP training is a marathon and not a sprint.
Merging academic theory with appropriate practice is a real challenge, especially during a global pandemic. We’ve all had to adapt to a new digital world of virtual meetings since the pandemic started and access to a university course (normally a practical course), is no exception. Lectures are currently being run via Zoom, which does make group discussions more challenging but, shared experiences with fellow trainee ANPs will be of help throughout my training, if only to act as a form of support. Access to university practical sessions are currently limited, increasing the need for further skills practice within a clinical setting. History taking and clinical examination skills can ideally be practiced safely in a variety of specialist hospital clinics under supervision, however, due to the current pandemic, many clinics are running a virtual service with specialist consultants assessing their patient needs via telephone or videophone.
I’ve attended several virtual and face-to-face clinics to date, and I am constantly amazed by the ability of NHS teams to provide new and creative solutions to the challenges faced by the pandemic. At one face-to-face clinic, a videophone was used to access a translator for a deaf couple, where sign language was used to take a clear history and plan a suitable treatment pathway.
All trainee ANPs are supported by a medical mentor who can help to support clinical knowledge and practice. I am fortunate that I have been able to discuss and practice some of my clinical examination skills, with my mentor, on research patients as part of the PHOSP COVID study, which is taking place at MFT and other trusts across the UK.
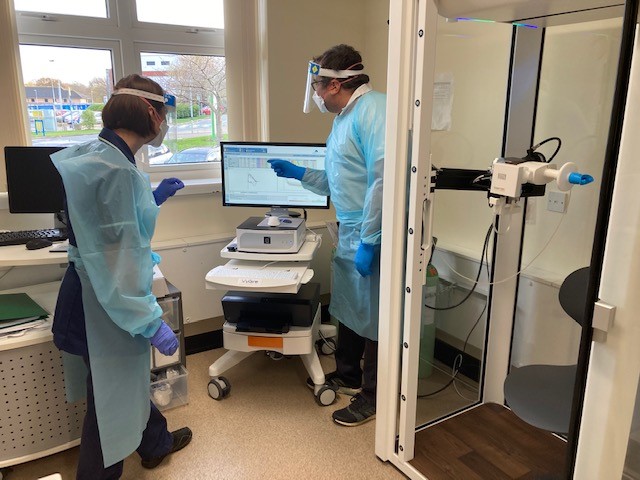
With the support of the physiologists at the CRF, I have been practising and developing my lung function testing skills. This includes learning to perform Diffusing Capacity Of The Lungs For Carbon Monoxide (DLCO) which tests oxygen transfer, and the level of fibrosing (scarring) in the lungs. These are skills needed to test specific respiratory conditions and this learning will also serve me well when I take up my upcoming respiratory elective module.

*Sue with physiologist Ian Waller learning to interpret DLCO respiratory test results
At some point, hopefully in the not too distant future, my training will be able to revert to more patient and colleague contact, but until then I am making the most of every potential training opportunity that I can find.
The ANP Role – Challenges in research
The ANP role can vary enormously depending on level of experience and area of speciality. As a new trainee ANP, there’s a clear challenge to both me and other healthcare professionals around me, to understanding the gradual development and full scope of this role. Taking part in this year’s virtual conference for advanced practitioners was a great start to understanding the large variety of ANPs nationally and the great work that they’re involved in. Additionally, I have reached out to several ANPs within MFT, in order to gain more understanding of the broad range of specialities and skills this role can deliver.
Spending time with ANPs across MFT has not only given me a great support network and encouragement but allowed me tremendous insight into what you can do as an ANP as I’ve seen how they’ve set up and delivered specialist services and pathways in their roles.

*Sue with research ANP Suja Subin
I have been able to spend time with Suja Subin, a research ANP within MFT, which has helped enormously with regards to how my role can develop and the challenges that I am likely to face.
The ANP role is so unique that I understand that there are less than 10 research ANPs in the country, so I am doing my part to raise the profile of the ANP research role where I can. This started with speaking to our own CRF team on how the change in my role will fit in with the CRF and the potential positive impact to our service delivery.

*Sue helping to raise the profile of the ANP research role
Over the next two years, I expect that my training to be an ANP in research will be challenging, however, it is clearly a fantastic opportunity for both my own personal development and the growth and service that the CRF can provide. I also hope that one day I might be in a position to help support and inspire the next generation of ANPs in the way I am being inspired and supported on this exciting journey.