Hearts, data and technology
How advances in technology and data from pacemakers are alerting doctors of heart failure patients who may benefit from medical attention.
Heart failure vs heart attacks
People often confuse heart failure with heart attacks. However, they are not the same thing. Heart attacks are caused by a sudden loss of blood supply to the heart, most commonly due to a blocked heart artery. In contrast, heart failure, which affects up to one million people in the UK, is a condition when the heart does not pump enough blood to meet the body’s needs.
What everyone should know about heart failure
Receiving a diagnosis of heart failure can be frightening. Although the description includes the word ‘failure’, it doesn’t mean that the heart is about to stop. Instead, it indicates that the heart, considered one of the hardest working muscles in the body, has become weakened and is not pumping properly.
Although heart failure often affects older people, it can occur at any age.
Damage to the heart muscle due to a previous heart attack may cause heart failure but there are many other causes, including high blood pressure, problems with the heart valves, viral infections and inherited heart conditions.
Heart Failure in the UK
Despite significant advances in treatment during the last decade, heart failure is a common reason for emergency admission to hospital, responsible for more than 100,000 admissions each year in the UK1.

While advances in heart failure therapies have reduced deaths due to heart failure by as much as 50 per cent, unfortunately, many patients do not live longer than five years.2 In view of this, early diagnosis and prompt effective treatment are critically important to stabilise the condition and ensure the best outcomes for people with heart failure.
Pacemakers, defibrillators and heart failure
In addition to medications, specialised pacemakers and defibrillator devices can be used in certain patients with heart failure to help the heart pump better and correct irregular heart rhythms. These devices are implanted in the chest, via a small incision just below the collarbone and are connected to the heart using electrical wires which sit inside the heart.
Once implanted, a defibrillator monitors every single heartbeat. If a dangerous heart rhythm is detected, then the device can deliver painless treatment by rapidly pacing the heart for a few seconds to terminate the abnormal rhythm. If the abnormal heart rhythm continues, then the defibrillator delivers one or more shocks to restart the heart.
Normally, the two sides of the heart beat at the same time. In many patients with heart failure, the two sides of the heart are out of synch. This can be improved by specialised pacemakers where, electrical impulses resynchronise the heart muscle to improve the pumping strength of the heart, relieving the symptoms of heart failure and prolonging life. In addition, these devices can monitor patients for early signs of deteriorating health.
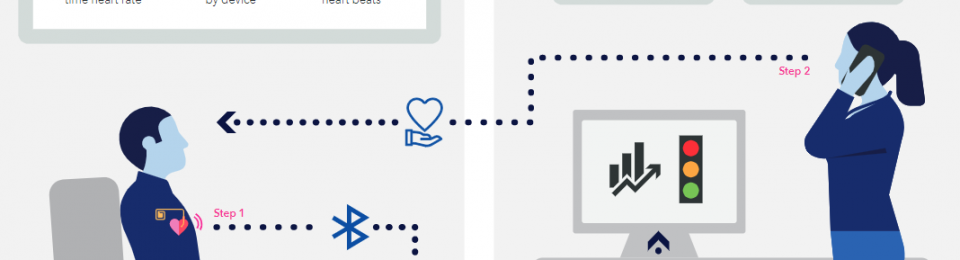
How Manchester specialists are identifying heart failure patients at risk of deteriorating
Led by Dr Fozia Ahmed – Consultant Cardiologist at Manchester Royal Infirmary, part of Manchester University NHS Foundation Trust (MFT) – heart failure specialists in Greater Manchester are making use of new monitoring technology in cardiac devices to identify patients, who left untreated, are at risk of being admitted to hospital. Alerts from specialist pacemakers and defibrillators are sent directly to the heart failure team, who then undertake a telephone assessment to deliver specialist care. In the majority of cases, this early intervention can potentially prevent patients requiring admission to hospital.
The new feature, known as TriageHF, created by the manufacturer (Medtronic), analyses data collected by the device such as heart rate, rhythm, fluid levels and physical activity to identify patients with deteriorating heart function. Devices can be linked to a patient’s smartphone or special home monitor which shares information directly with the hospital team.
Once the specialist hospital team assesses the patient, they can act immediately to prescribe or adjust medications, arrange tests, give advice, or ask the patient to come in if required.

Results of a two-year clinical study, involving more than 400 patients, showed that using health-related data from heart devices in this new way can significantly cut the risk of hospitalisation by identifying high risk patients whose fluid levels in the lungs had increased or whose heart beats had become irregular. Patients under the care of the new service, which utilised pacemaker data to guide treatment, experienced a reduction in cardiovascular hospital admissions, associated with receiving the additional care.3 Dr Camilla Sammut-Powell, a medical statistician from The University of Manchester, added that information provided by the patient’s device in real-time may be used by heart care teams to ensure that the patient is receiving therapies designed to improve their condition and long-term prognosis.
Who stands to benefit?
There are approximately 30,000 patients in the UK who have this type of cardiac device, but most do not currently have the monitoring function switched on. This new research has led to more heart centres activating this new technology to improve patient care and avoiding hospital admissions.
Dr Joanne Taylor, British Heart foundation Clinical Research Fellow, based at MFT and The University of Manchester, who specialises in medicine for older people, added:
Heart failure typically waxes and wanes, with spells of worsening fluid retention. Caught early, these spells can often be easily managed by changes to medication, however if missed can lead to hospitalisation if fluid accumulates in the lungs or specialist monitoring is required.
Patients with heart failure usually have a check up with a specialist every six to 12 months, but this isn’t always frequent enough to spot the sudden decline that can happen in between scheduled appointments.

Heart Failure: Improving lives with data
Before this new technology, heart teams relied on the patient getting in contact if they began to feel unwell in between their hospital appointments. This new technology takes a different approach, providing continuous monitoring of health information from patients’ pacemakers and defibrillators and directly notifying specialist heart failure nurses and doctors if signs of deterioration are detected. This allows them to treat patients at home before they become unwell, avoiding admission to hospital.
Dr Ahmed added: “Heart failure is responsible for more than 100,000 hospital admissions each year in the UK, but with early detection and prompt treatment, many of these admissions are potentially avoidable. How we practice requires radical reform. Technology doesn’t stand still, and neither should healthcare. Thanks to advances in cardiac device technology, we are now in a much stronger position to monitor, manage and care for patients in ways that I would have never thought possible.
TriageHF allows us to quickly identify unstable patients and deliver specialist care to patients in a home environment, at times of clinical need when they may be unwell.
“By combining the health-related data from the pacemaker alert with information provided by patients over the phone, we are able to determine whether a patient requires a change in treatment or needs to be reviewed in person.”